For Health Plan and TPA leaders, the regulatory era of transparency has set the stage for a competitive battleground. Compliance alone was never a differentiation strategy. To truly compete in the market and gain a competitive edge, price transparency data must be expertly curated, integrated, and delivered. TALON’s platform transforms raw machine-readable file (MRF) data into actionable, member-specific intelligence. With unmatched accuracy, real-time updates, intuitive shopping solution, and embedded rewards, TALON enables plans to improve member trust, reduce out-of-network leakage, and achieve measurable cost savings, all while maintaining airtight, guaranteed compliance.
Executive Summary
- Who this is for: Health Plan and TPA leaders navigating healthcare consumerism, affordability concerns, and transparency compliance.
- The challenge: Meeting Transparency in Coverage (TiC) and No Surprises Act requirements while driving adoption and savings.
- The TALON edge: Curated price transparency built on real MRF intelligence, integrated workflows, and behavioral economics.
- Top outcomes: Higher tool engagement, improved access and affordability, and increased member trust and satisfaction.
- Next step: Request a 30-minute executive briefing or ROI model demo.
The Business Problem
Health plans and TPAs face a convergence of pressures: regulatory scrutiny, member cost frustration and confusion, and administrative fatigue from fragmented systems. Many transparency tools fail to deliver value because they rely on incomplete or outdated data, offer generic cost ranges, or create friction in member workflows.
This results in low adoption, poor steerage, and rising leakage which means members either don’t use the tools or don’t trust them.
Curated transparency reverses this equation: when data is accurate, contextual, and integrated, members make smarter choices. Enable an outcome loop that scales via better decisions that drive measurable reductions in spend and higher satisfaction.
Why Curated Price Transparency Matters Now
“Curated” transparency is more than data access. It’s data mastery.
To be curated, a system must combine:
- Accuracy – contract-rate fidelity and MRF-validated encounter costs
- Completeness – all covered and shoppable services, not just the top 500
- Timeliness – dynamic monthly updates as MRFs change
- Explainability – clear, member-friendly language showing what costs mean
- Usability – frictionless experience at the point of care or scheduling
Common pitfalls of basic solutions, like ghost rates, stale data, and narrow service sets, undermine trust and engagement. Plans that adopt curated transparency move from compliance checklists to member-centric engagement.
Curated transparency is not about showing prices. It enables health plans and TPAs to show confidence in the value your network delivers.
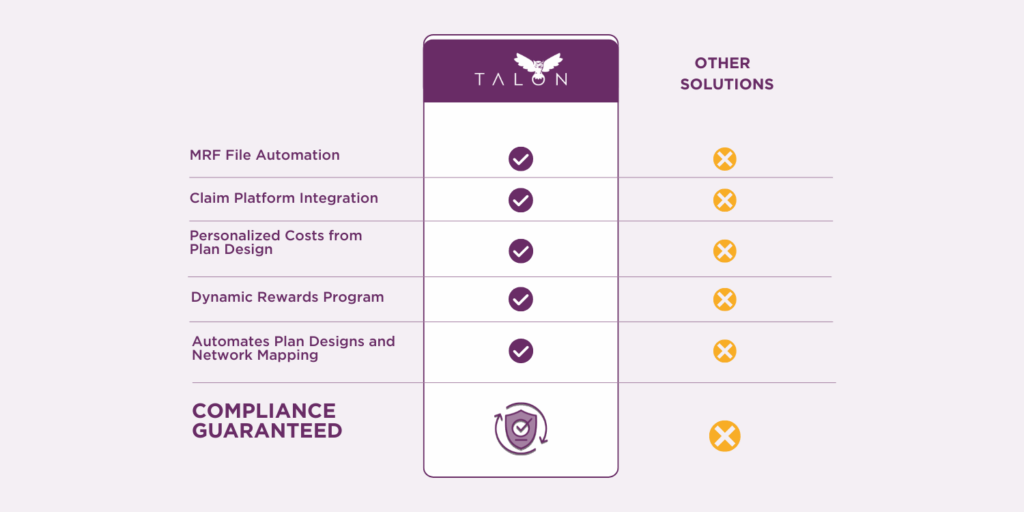
TALON’s Competitive Advantage: Curated Price Transparency
Pillar 1 – Data and Accuracy
TALON’s 12-step data curation and back-testing process eliminates ghost and zombie rates, validating all in-network negotiated prices from machine-readable files.
- Reflects real contract rates and benefit accumulators.
- Generates complete encounter estimates, not fragmented line items.
Impact: Higher trust, fewer surprise bills, and better steerage.
Pillar 2 – Usability and Adoption
A fully responsive, mobile-first interface with plain-language cost breakdowns helps members understand total cost of care.
- “No Surprise Shopping” encounter estimates clarify all components.
- Behavioral nudges and integrated MyMedicalRewards™ incentives drive sustained engagement.
Result: Meaningful adoption growth; 15-20% lift in member engagement.
Pillar 3 – Integration and Workflow
Deep API, SSO, and claims platform integration ensures pricing aligns with real benefit design and accumulators.
- Compatible with portals, digital front doors, and care navigation systems.
- Embedded support dashboards enable user impersonation and utilization monitoring for administrators.
Outcome: Seamless operations with measurable productivity gains.
Pillar 4 – Compliance as Baseline, Strategy as Differentiator
TALON doesn’t stop at compliance. It turns TiC and No Surprises Act data into a strategic advantage—supporting QPA calculation, direct contracting, and dynamic network mapping.
Benefit: Plans can innovate faster and launch new consumer-friendly products in weeks, not months.
Outcomes and ROI: A Directional Model
The ROI equation is simple:
More adoption → better steerage → lower unit costs → fewer member escalations.
If transparency tool adoption increases from 15% to 35%, and in-network steerage via incentive-driven tools improves by 5–7 percentage points, the projected savings could reach 4x of license fees within 12 months, depending on network mix and baseline spend.
Beyond savings, plans see measurable gains in member satisfaction, reduced churn, and stronger fiduciary support.
Risks of Inaction
Plans that delay adopting curated transparency face:
- Low member engagement due to untrusted, non-personalized data.
- Compliance exposure as CMS enforcement intensifies.
- Missed steerage savings from members defaulting to high-cost providers.
- Brand erosion as competitors launch more consumer-friendly tools.
What You’ll Gain with TALON
- Real-time, compliant member pricing for all covered items and services.
- 15-20% improvement in transparency tool utilization.
- Configurable incentives aligned with plan objectives.
- End-to-end integration with existing claims platforms.
- Measurable internal efficiency gains with administrative dashboards capabilities.
Book a Strategy Session to transform compliance into growth and discover why leading health plans and TPAs trust TALON to make transparency work for their members and their bottom line.
